






 james thomas -
9 hours ago -
Health -
27 views -
0 Comments -
0 Likes -
0 Reviews
james thomas -
9 hours ago -
Health -
27 views -
0 Comments -
0 Likes -
0 Reviews
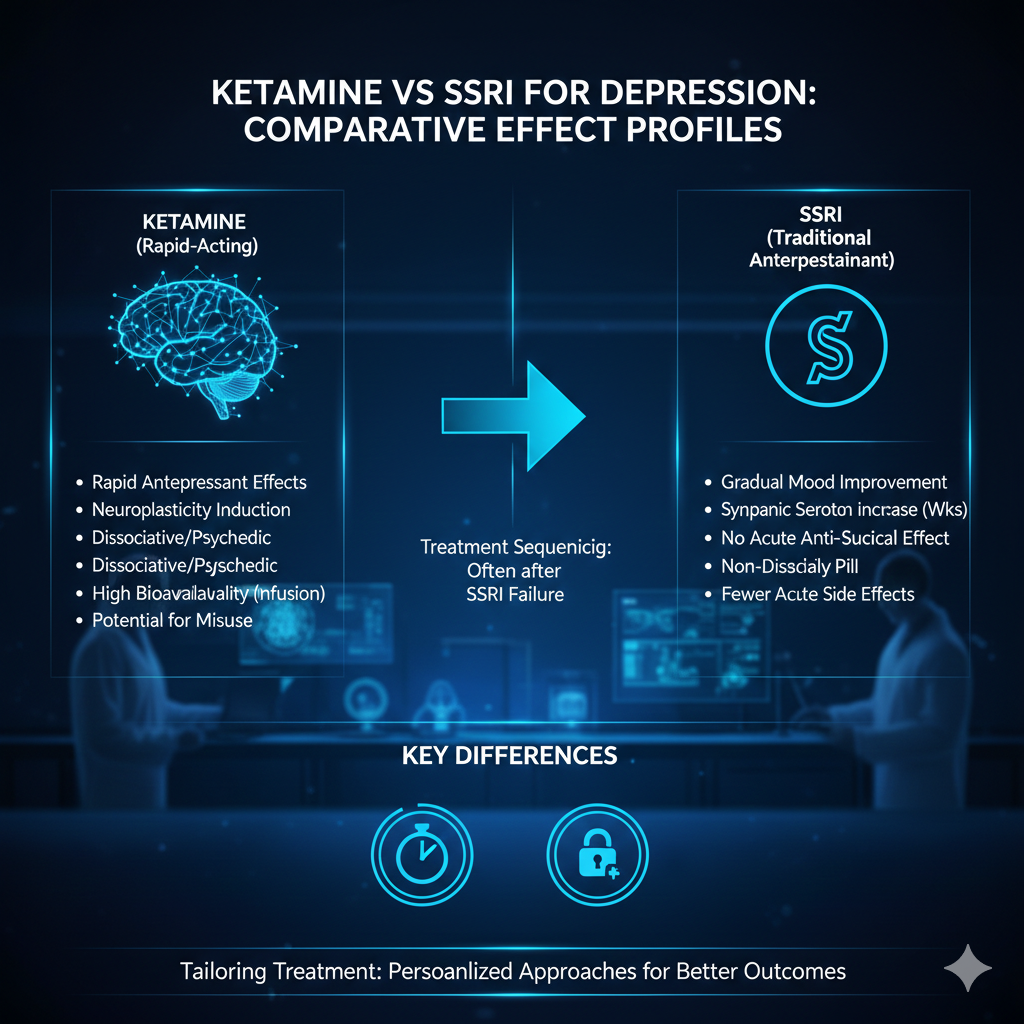
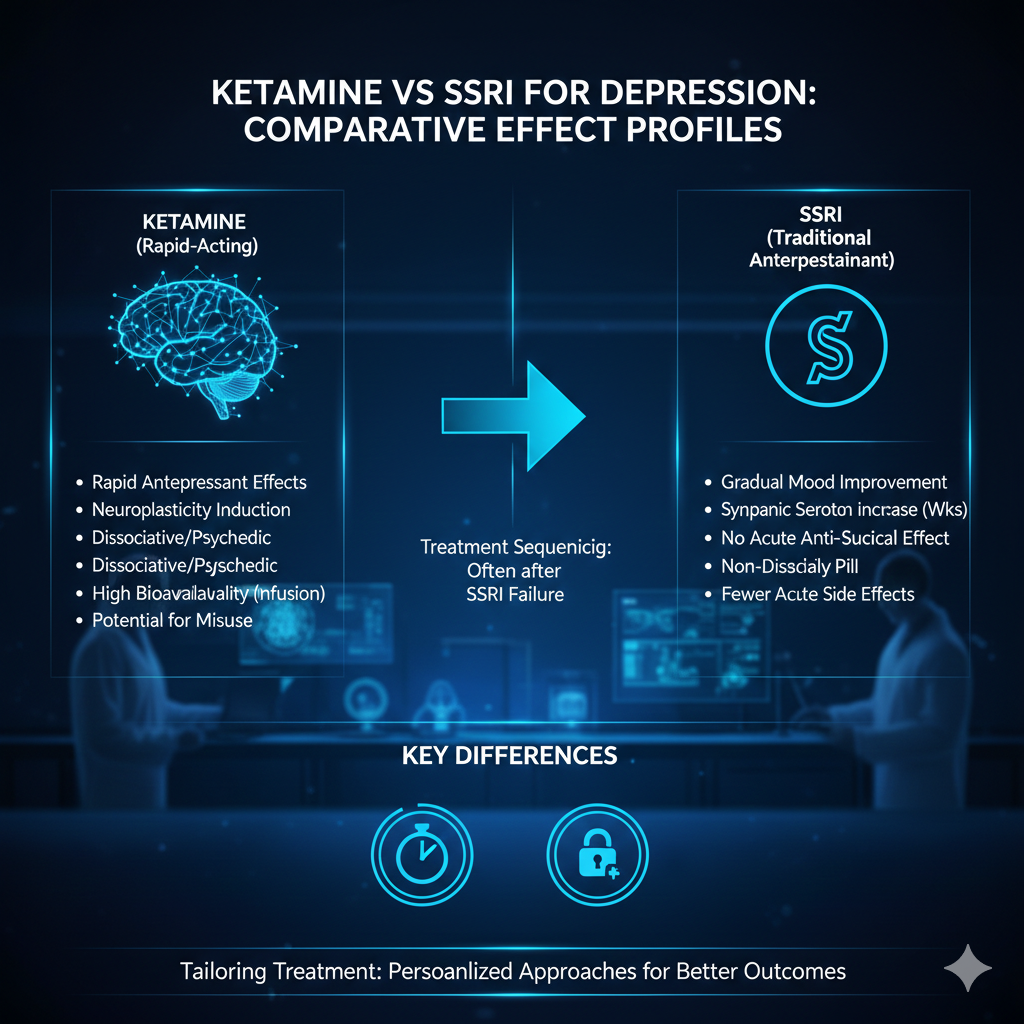
Depression is one of the most prevalent mental health disorders, and finding the right treatment is essential for improving patients’ quality of life. Ketamine vs SSRI (selective serotonin reuptake inhibitors) is a commonly debated comparison when it comes to effective depression management. While SSRIs have long been the go-to treatment for depression, ketamine has recently emerged as a promising alternative, particularly for patients with treatment-resistant depression (TRD). In this article, we’ll compare the effect profiles of ketamine vs SSRI, their mechanisms of action, and the optimal sequencing of these treatments for patients.
Selective serotonin reuptake inhibitors (SSRIs) are among the most commonly prescribed antidepressants worldwide. SSRIs, including fluoxetine (Prozac), sertraline (Zoloft), and escitalopram (Lexapro), work by increasing serotonin levels in the brain. Serotonin is a neurotransmitter that regulates mood, and by blocking its reuptake, SSRIs help increase the amount of serotonin available to the brain. This process is believed to improve mood and alleviate depressive symptoms.
SSRIs are often effective in treating mild to moderate depression, with a typical onset of action that can take 4 to 6 weeks. For most patients, SSRIs are well-tolerated, with side effects like nausea, weight gain, and sexual dysfunction being common but not severe. However, SSRIs can be less effective in patients with treatment-resistant depression whose symptoms do not improve after trying multiple antidepressants or other therapies.
SSRIs are typically considered the first-line treatment for depression due to their established safety and efficacy profile. However, the time it takes for SSRIs to show results can be a significant drawback for patients in acute distress. For those who do not respond to SSRIs or experience intolerable side effects, other treatments may be necessary.
In contrast to SSRIs, ketamine has emerged as a rapid-acting alternative, particularly for individuals with treatment-resistant depression. Originally developed as an anesthetic, ketamine has demonstrated powerful antidepressant effects when used in sub-anesthetic doses. It works by targeting NMDA receptors in the brain, which are involved in glutamate transmission, a neurotransmitter that plays a critical role in mood regulation.
Unlike SSRIs, ketamine offers rapid relief from depressive symptoms, often within hours or days after administration. This rapid onset of action is especially important for patients who need immediate relief from suicidal ideation or severe depressive symptoms. Ketamine also has a different mechanism of action compared to SSRIs, making it particularly effective for patients who have not responded to traditional antidepressants.
While ketamine is available in various forms, including intravenous (IV) infusions, intranasal spray (SPRAVATO®), and oral tablets or troches, the most well-studied and clinically used forms are IV and intranasal. Studies have shown that ketamine can provide lasting benefits, but its effects are often short-term and may require repeat treatments to maintain symptom relief.
When comparing ketamine vs SSRI for depression, several key differences in their effect profiles emerge. Below, we’ll examine these differences in terms of onset of action, efficacy, duration of effect, and safety.
In many cases, ketamine and SSRIs can complement each other rather than being used as alternatives. The optimal sequencing for these treatments depends on the patient’s specific needs and the severity of their depression.
The debate of ketamine vs SSRI for depression comes down to the individual needs of the patient. SSRIs have long been the cornerstone of depression treatment due to their proven efficacy and safety, but they may not work for everyone, particularly in cases of treatment-resistant depression. On the other hand, ketamine offers a promising alternative with rapid symptom relief but may require repeat treatments to maintain its benefits.
For patients with severe or treatment-resistant depression, ketamine can serve as a powerful tool, while SSRIs remain an essential part of long-term depression management. By understanding the comparative effect profiles and appropriate treatment sequencing, healthcare providers can offer a more personalized and effective approach to managing depression, giving patients the best chance at recovery.

This website uses cookies to ensure you get the best experience on our website.
To learn more about our privacy policy Click here